Prostate cancer is cancer of the small walnut-shaped gland in males that produces seminal fluid, the fluid that nourishes and transports sperm. Prostate cancer is one of the most common types of cancer in men, affecting about one in six men in the United States. A diagnosis of prostate cancer can be scary not only because it can be life-threatening, but also because treatments can cause side effects such as bladder control problems and erectile dysfunction (impotence). But diagnosis and treatment of prostate cancer have gotten much better in recent years.
Prostate cancer usually grows slowly and initially remains confined to the prostate gland, where it may not cause serious harm. While some types of prostate cancer grow slowly and may need minimal or no treatment, other types are aggressive and can spread quickly. If prostate cancer is detected early — when it's still confined to the prostate gland — you have a better chance of successful treatment.
Symptoms
Prostate cancer usually doesn't produce any noticeable symptoms in its early stages, so many cases of prostate cancer aren't detected until the cancer has spread beyond the prostate. For most men, prostate cancer is first detected during a routine screening such as a prostate-specific antigen (PSA) test or a digital rectal exam (DRE).
When signs and symptoms do occur, they depend on how advanced the cancer is and how far the cancer has spread.
Early signs and symptoms of prostate cancer can include urinary problems, caused when the prostate tumor presses on the bladder or on the tube that carries urine from the bladder (urethra). However, urinary symptoms are much more commonly caused by benign prostate problems, such as an enlarged prostate (benign prostatic hyperplasia) or prostate infections. Less than 5 percent of cases of prostate cancer have urinary problems as the initial symptom. When urinary signs and symptoms do occur, they can include:
* Trouble urinating
* Starting and stopping while urinating
* Decreased force in the stream of urine
Cancer in your prostate or the area around the prostate can cause:
* Blood in your urine
* Blood in your semen
Prostate cancer that has spread to the lymph nodes in your pelvis may cause:
* Swelling in your legs
* Discomfort in the pelvic area
Advanced prostate cancer that has spread to your bones can cause:
* Bone pain that doesn't go away
* Bone fractures
* Compression of the spine
Causes
Cancer is a group of abnormal cells that grow more rapidly than normal cells and that refuse to die. Cancer cells also have the ability to invade and destroy normal tissues, either by growing directly into surrounding structures or after traveling to another part of your body through your bloodstream or lymph system (metastasize). Microscopic cancer cells develop into small clusters that continue to grow, becoming more densely packed and hard.
What causes prostate cancer and why some types behave differently are unknown. Research suggests that a combination of factors may play a role, including heredity, ethnicity, hormones, diet and the environment.
Risk factors
Knowing the risk factors for prostate cancer can help you determine if and when you want to begin prostate cancer screening. The main risk factors include:
* Age. After age 50, your chance of having prostate cancer increases.
* Race or ethnicity. For reasons that aren't well understood, black men have a higher risk of developing and dying of prostate cancer.
* Family history. If your father or brother has prostate cancer, your risk of the disease is greater than that of the average man.
* Diet. A high-fat diet and obesity may increase your risk of prostate cancer. One theory is that fat increases production of the hormone testosterone, which may promote the development of prostate cancer cells.
* High testosterone levels. Because testosterone naturally stimulates the growth of the prostate gland, men who use testosterone therapy are more likely to develop prostate cancer than are men who have lower levels of testosterone. Also, doctors are concerned that testosterone therapy might fuel the growth of prostate cancer that is already present. Long-term testosterone treatment also may cause prostate gland enlargement (benign prostatic hyperplasia).
When to seek medical advice
If you have difficulties with urination, see your doctor. This condition doesn't always relate to prostate cancer, but it can be a sign of prostate-related problems.
Beginning at age 50, the American Cancer Society recommends having yearly screening tests for prostate cancer. If you're black or have a family history of the disease, you may want to begin at a younger age. Yearly screenings can help detect prostate cancer early, when it's easier to treat. They include:
* PSA test. This blood test checks levels of prostate-specific antigen (PSA), which can be a sign of prostate cancer. While this test can detect signs of cancer, elevated PSA levels are sometimes caused by conditions other than cancer, such as prostate enlargement, infection or inflammation.
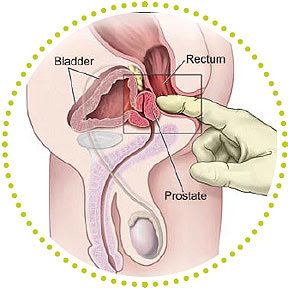
* Digital rectal exam (DRE). This test involves insertion of a lubricated finger into the rectum to feel for bumps on the prostate. While it can be slightly uncomfortable, an annual DRE is a quick, simple exam that can be a lifesaver.
Tests and diagnosis
Prostate cancer may not cause any symptoms at first. The first indication of a problem may come during a routine screening test, such as:
* Digital rectal exam (DRE). During a DRE, your doctor inserts a gloved, lubricated finger into your rectum to examine your prostate, which is adjacent to the rectum. If your doctor finds any abnormalities in the texture, shape or size of your gland, you may need more tests.
* Prostate-specific antigen (PSA) test. A blood sample is drawn from a vein and analyzed for PSA, a substance that's naturally produced by your prostate gland to help liquefy semen. It's normal for a small amount of PSA to enter your bloodstream. However, if a higher than normal level is found, it may be an indication of prostate infection, inflammation, enlargement or cancer. Studies have not been able to show that routine screening decreases the chance that anyone will die of prostate cancer, but screening with PSA and DRE can help identify cancer at an earlier stage.
* Transrectal ultrasound. If other tests raise concerns, your doctor may use transrectal ultrasound to further evaluate your prostate. A small probe, about the size and shape of a cigar, is inserted into your rectum. The probe uses sound waves to get a picture of your prostate gland.
* Prostate biopsy. If initial test results suggest prostate cancer, your doctor may recommend biopsy. To do a prostate biopsy, your doctor inserts a small ultrasound probe into your rectum. Guided by images from the probe, your doctor uses a fine, spring-propelled needle to retrieve several very thin sections of tissue from your prostate gland. A pathologist who specializes in diagnosing cancer and other tissue abnormalities evaluates the samples. From those, the pathologist can tell if the tissue removed is cancerous and estimate how aggressive your cancer is.
Determining how far the cancer has spread
Once a cancer diagnosis has been made, you may need further tests to help determine if or how far the cancer has spread. Many men don't require additional studies and can directly proceed with treatment based on the characteristics of their tumors and the results of their pre-biopsy PSA tests.
* Bone scan. A bone scan takes a picture of your skeleton in order to determine whether cancer has spread to the bone. Prostate cancer can spread to any bones in your body, not just those closest to your prostate, such as your pelvis or lower spine.
* Ultrasound. Ultrasound not only can help indicate if cancer is present, but also may reveal whether the disease has spread to nearby tissues.
* Computerized tomography (CT) scan. A CT scan produces cross-sectional images of your body. CT scans can identify enlarged lymph nodes or abnormalities in other organs, but they can't determine whether these problems are due to cancer. Therefore, CT scans are most useful when combined with other tests.
* Magnetic resonance imaging (MRI). This type of imaging produces detailed, cross-sectional images of your body using magnets and radio waves. An MRI can help detect evidence of the possible spread of cancer to lymph nodes and bones.
* Lymph node biopsy. If enlarged lymph nodes are found by a CT scan or an MRI, a lymph node biopsy can determine whether cancer has spread to nearby lymph nodes. During the procedure, some of the nodes near your prostate are removed and examined under a microscope to determine if cancerous cells are present.
Grading
When a biopsy confirms the presence of cancer, the next step, called grading, is to determine how aggressive the cancer is. The tissue samples are studied, and the cancer cells are compared with healthy prostate cells. The more the cancer cells differ from the healthy cells, the more aggressive the cancer and the more likely it is to spread quickly.
Cancer cells may vary in shape and size. Some cells may be aggressive, while others aren't. The pathologist identifies the two most aggressive types of cancer cells when assigning a grade. The most common scale used to evaluate prostate cancer cells is called a Gleason score. Based on the microscopic appearance of cells, individual ratings from 1 to 5 are assigned to the two most common cancer patterns identified. These two numbers are then added together to determine your overall score. Scoring can range from 2 (nonaggressive cancer) to 10 (very aggressive cancer).
Staging
After the level of aggressiveness of your prostate cancer is known, the next step, called staging, determines if or how far the cancer has spread. Your cancer is assigned one of four stages, based on how far it has spread:
* Stage I. Signifies very early cancer that's confined to a microscopic area that your doctor can't feel.
* Stage II. Your cancer can be felt, but it remains confined to your prostate gland.
* Stage III. Your cancer has spread beyond the prostate to the seminal vesicles or other nearby tissues.
* Stage IV. Your cancer has spread to lymph nodes, bones, lungs or other organs.
Complications
Complications from prostate cancer are related to both the disease and its treatment. One of the biggest fears of many men who have prostate cancer is that treatment may leave them incontinent or unable to maintain an e******n firm enough for sex (erectile dysfunction). Fortunately, therapies exist to help cope with or treat these conditions.
The typical complications of prostate cancer and its treatments include:
* Spread of cancer. Prostate cancer can spread to nearby organs or travel through your bloodstream or lymphatic system, affecting your bones or other organs. Treatments for prostate cancer that has spread can include hormone therapy, radiation therapy and chemotherapy.
* Pain. Although early-stage prostate cancer typically isn't painful, once it's spread to bones it can be. Not all people with cancer that has spread to bones have pain, but in some cases, pain is intense and doesn't go away. Treatments directed at shrinking the cancer often can produce significant pain relief. Medications ranging from over-the-counter pain relievers to prescription narcotics can alleviate pain. If your pain is severe, you may need to see a pain specialist. While it's not always possible to make all of your pain go away, your doctor will work with you to try to control pain to a point where you're comfortable. If you're in serious pain, tell your doctor. Pain can be controlled, and there's no reason you have to suffer.
* Difficulty urinating (urinary incontinence). Both prostate cancer and its treatment can cause incontinence. Treatment depends on the type of incontinence you have, how severe it is and the likelihood it will improve over time. Treatments include behavior modifications (such as going to the bathroom at set times rather than just according to urges), exercises to strengthen pelvic muscles (commonly called Kegel exercises), medications and catheters. If incontinence continues for a prolonged period without getting better, your doctor may suggest more aggressive procedures. These may include implanting an artificial urinary sphincter, placement of a sling of synthetic material to compress the urethra, or the injection of bulking agents into the lining of the urethra at the base of the bladder to reduce leakage.
* Erectile dysfunction (ED) or impotence. Like incontinence, ED can be a result of prostate cancer or its treatment, including surgery, radiation or hormone treatments. Medications and vacuum devices that assist in achieving e******n are available to treat ED. Medications include sildenafil (Viagra), tadalafil (Cialis) and vardenafil (Levitra). If other treatments fail, penile implants can be inserted surgically to help create an e******n.
* Depression. Many men may feel depressed after a diagnosis of prostate cancer or after trying to cope with the side effects of treatment. These feelings may last for only a short time, they may come and go, or they may linger for weeks or even months. Talk to your doctor if you have depression that interferes with your ability to get things done or enjoy your life. Treatment such as counseling or antidepressant medication can make a big difference.
Treatments and drugs
There's more than one way to treat prostate cancer. For some men a combination of treatments — such as surgery followed by radiation or radiation paired with hormone therapy — works best. The treatment that's best for each man depends on several factors. These include how fast your cancer is growing, how much it has spread, your age and life expectancy, as well as the benefits and the potential side effects of the treatment. The most common treatments for prostate cancer include the following:
External beam radiation therapy (EBRT)
External beam radiation treatment uses high-powered X-rays to kill cancer cells. This type of radiation is effective at destroying cancerous cells, but it can also scar adjacent healthy tissue.
The first step in radiation therapy is to map the precise area of your body that needs to receive radiation. Computer-imaging software helps your doctor find the best angles to aim the beams of radiation. Precisely focused radiation kills cancer in your prostate while minimizing harm to surrounding tissue.
Treatments are generally given five days a week for about eight weeks. Each treatment appointment takes about 10 minutes. However, much of this is preparation time — radiation is received for only about one minute. You don't need anesthesia with external beam radiation, because the treatment isn't painful.
You'll be asked to arrive for therapy with a full bladder. This will push most of your bladder out of the path of the radiation beam. A body supporter holds you in the same position for each treatment. Ink marks on your skin help guide the radiation beam, and small gold markers may be placed in your prostate to ensure the radiation hits the same targets each time. Custom-designed shields help protect nearby normal tissue, such as your bladder, erectile tissues, anus and rectal wall.
EBRT can cause mild side effects, but in most cases they disappear shortly after your course of treatment is finished.
Side effects of EBRT can include:
* Urinary problems. The most common signs and symptoms are urgency to urinate and frequent urination. These problems usually are temporary and gradually diminish in a few weeks after completing treatment. Long-term problems are uncommon.
* Loose stools, rectal bleeding, discomfort during bowel movements or a sense of needing to have a bowel movement (rectal urgency). In some cases these problems persist for months after treatment, but they improve on their own in most men. If you do have long-term rectal symptoms, medications can help. Rarely, men develop persistent bleeding or a rectal ulcer after radiation. Surgery may be necessary to alleviate these problems.
* Sexual side effects. Radiation therapy doesn't usually cause immediate sexual side effects such as erectile dysfunction, but some men who've had the treatment have sexual problems later in life.
Radioactive seed implants
Radioactive seeds implanted into the prostate have gained popularity in recent years as a treatment for prostate cancer. The implants, also known as brachytherapy, deliver a higher dose of radiation than do external beams, but over a substantially longer period of time. The therapy is generally used in men with smaller or moderate-sized prostates with small and lower grade cancers.
During the procedure, between 40 and 100 rice-sized radioactive seeds are placed in your prostate through ultrasound-guided needles. The implant procedure typically lasts one to two hours and is done under general anesthesia — which means you won't be awake. Most men can go home the day of the procedure. Sometimes, hormone therapy is used for a few months to shrink the size of the prostate before seeds are implanted. The seeds may contain one of several radioactive isotopes — including iodine and palladium. These seeds don't have to be removed after they stop emitting radiation. Iodine and palladium seeds generally emit radiation that extends only a few millimeters beyond their location. This type of radiation isn't likely to escape your body in significant doses. However, doctors recommend that for the first few months you stay at least six feet (1.83 meters) away from children and pregnant women, who are especially sensitive to radiation. All radiation inside the pellets is generally exhausted within a year.
Side effects of radioactive seed implants can include:
* Urinary problems. The procedure causes urinary signs and symptoms such as frequent, slow and painful urination in nearly all men. You may require medication to treat these signs and symptoms. Some men need medications or the use of intermittent self-catheterization to help them urinate. Urinary symptoms tend to be more severe and longer lasting with seed implants than with external beam radiation.
* Sexual problems. Some men experience erectile dysfunction due to radioactive seed implants.
* Rectal symptoms. Sometimes this treatment causes loose stools, discomfort during bowel movements or other rectal symptoms. However, rectal symptoms from radioactive seed implants are generally less severe than with external beam radiation.
Hormone therapy
Hormone therapy involves trying to stop your body from producing the male sex hormones testosterone, which can stimulate the growth of cancer cells. This type of therapy can also block hormones from getting into cancer cells. Sometimes doctors use a combination of drugs to achieve both. In most men with advanced prostate cancer, this form of treatment is effective in helping both shrink the cancer and slow the growth of tumors. Sometimes doctors use hormone therapy in early-stage cancers to shrink large tumors so that surgery or radiation can remove or destroy them more easily. In some cases, hormone therapy is used in combination with radiation therapy or surgery. After these treatments, the drugs can slow the growth of any stray cancer cells left behind.
Some drugs used in hormone therapy decrease your body's production of testosterone. The hormones — known as luteinizing hormone-releasing hormone (LH-RH) agonists — can set up a chemical blockade. This blockade prevents the testicles from receiving messages to make testosterone. Drugs typically used in this type of hormone therapy include leuprolide (Lupron, Viadur) and goserelin (Zoladex). They're injected into a muscle or under your skin once every three or four months. You can receive them for a few months, a few years or the rest of your life, depending on your situation.
Other drugs used in hormone therapy block your body's ability to use testosterone. A small amount of testosterone comes from the adrenal glands and isn't suppressed by LH-RH agonists. Certain medications — known as anti-androgens — can prevent testosterone from reaching your cancer cells. Examples include bicalutamide (Casodex) and nilutamide (Nilandron). They come in tablet form and, depending on the particular brand of drug, are taken orally one to three times a day. These drugs typically are given along with an LH-RH agonist.
Simply depriving prostate cancer of testosterone usually doesn't kill all of the cancer cells. Within a few years, the cancer often learns to thrive without testosterone. Once this happens, hormone therapy is less likely to be effective. However, several treatment options still exist. To avoid such resistance, intermittent hormone therapy programs have been developed. During this type of therapy, the hormonal drugs are stopped after your PSA drops to a low level and remains steady. You will need to resume taking the drugs if your PSA level rises again.
Side effects of hormone therapy can include:
* Breast enlargement (gynecomastia)
* Reduced sex drive
* Erectile dysfunction
* Hot flashes
* Weight gain
* Reduction in muscle and bone mass
Certain hormone therapy medications can also cause:
* Nausea
* Diarrhea
* Fatigue
* Liver damage
Recent reports have shown that men who undergo hormone therapy for prostate cancer may have a higher risk of having a heart attack in the first year or two after starting hormone therapy. So your doctor should carefully monitor your heart condition and aggressively treat any other conditions that may predispose you to a heart attack, such as high blood pressure, high cholesterol or smoking.
Surgery to remove the testicles, which produce most of your testosterone, is as effective as other forms of hormonal therapy. Many men are not comfortable with the idea of losing their testicles, so they opt for the above-noted methods of lowering testosterone in the body. However, removing the testicles has the advantage of not having to have an injection every three or four months and can be less expensive. The surgery can be done on an outpatient basis using a local anesthetic.
Radical prostatectomy
Surgical removal of your prostate gland, called radical prostatectomy, is used to treat cancer that's confined to the prostate gland. During this procedure, your surgeon uses special techniques to completely remove your prostate and nearby lymph nodes. This surgery can affect muscles and nerves that control urination and sexual function. Two surgical approaches are available for a prostatectomy — retropubic surgery and perineal surgery.
* Retropubic surgery. The gland is taken out through an incision in your lower abdomen that typically runs from just below the navel to an inch (2.54 centimeters) above the base of the pen*s. It's the most commonly used form of prostate removal for two reasons. First, your surgeon can use the same incision to remove pelvic lymph nodes, which are tested to determine if the cancer has spread. Second, the procedure gives your surgeon good access to your prostate, making it easy to save the nerves that help control bladder function and erections.
* Perineal surgery. An incision is made between your anus and scrotum. There's generally less bleeding with perineal surgery, and recovery time may be shorter, especially if you're overweight. With this procedure, your surgeon isn't able to remove nearby lymph nodes.
During either type of operation, a catheter is inserted into your bladder through your pen*s to drain urine from the bladder during your recovery. The catheter will likely remain in place for one to two weeks after the operation while the urinary tract heals.
Side effects of radical prostatectomy can include:
* Bladder control problems (urinary incontinence). These symptoms can last for weeks or even months, but most men eventually regain bladder control. Many men experience stress incontinence, meaning they're unable to hold urine flow when their bladders are under increased pressure. This can happen when you sneeze, cough, laugh or lift something heavy. In some men, urinary incontinence doesn't get better and surgery is needed to help correct the problem.
* Erectile dysfunction. This is a common side effect of radical prostatectomy, because nerves on both sides of your prostate that control erections may be damaged or removed during surgery. Most men younger than age 50 who have nerve-sparing surgery are able to achieve erections afterward, and even some men in their 70s are able to maintain normal sexual functioning. Men who had trouble achieving or maintaining an e******n before surgery have a higher risk of being impotent after the surgery.
Robot-assisted laparoscopic radical prostatectomy (RALRP)
This is a relatively new procedure for removing the prostate. For robot-assisted laparoscopy, five small incisions are made in the abdomen through which the doctor inserts tube-like instruments, including a long, slender tube with a small camera on the end (laparoscope). This creates a magnified view of the surgical area.
The instruments are attached to a mechanical device, and the surgeon sits at a console and guides the instruments through a viewing device to perform the surgery. So far, studies show that traditional open prostatectomy and robotic prostatectomy have had similar outcomes related to cancer-free survival rates, urinary continence and sexual function one year after surgery. Longer term outcomes are not yet known.
Watchful waiting
The PSA blood test can help detect prostate cancer at a very early stage. This allows many men to choose watchful waiting as a treatment option. In watchful waiting (also known as observation, expectant therapy or deferred therapy), regular follow-up blood tests, rectal exams and possibly biopsies may be performed to monitor progression of your cancer.
During watchful waiting no medical treatment is provided. Medications, radiation and surgery aren't used. Watchful waiting may be an option if your cancer isn't causing symptoms, is expected to grow very slowly, and is small and confined to one area of your prostate.
Watchful waiting may be particularly appropriate if you're elderly, in poor health or both. Many such men will live out their normal life spans without treatment and without the cancer spreading or causing other problems. But watchful waiting can also be a rational option if you're a younger man, as long as you know the facts, are willing to be vigilant, and accept the risk of a tumor spreading during the observation period, rendering your cancer incurable.
Chemotherapy
This type of treatment uses chemicals that destroy rapidly growing cells. Chemotherapy can be quite effective in treating prostate cancer, but it can't cure it. Because it has more side effects than hormone therapy does, chemotherapy is reserved for men who have hormone-resistant prostate cancer that has spread to other parts of the body.
Cryotherapy
This treatment is used to destroy cells by freezing tissue. Original attempts to treat prostate cancer with cryotherapy involved inserting a probe into the prostate through the skin between the rectum and the scrotum (perineum). Using a rectal microwave probe to monitor the procedure, the prostate was frozen in an attempt to destroy cancer cells. This method often resulted in damage to tissue around the bladder and long-term complications such as injury to the rectum or the muscles that control urination.
More recently, smaller probes and more-precise methods of monitoring the temperature in and around the prostate have been developed. These advances may decrease the complications associated with cryotherapy, making it a more effective treatment for prostate cancer. Although progress continues, more time is needed to determine how successful cryotherapy may be as a treatment for prostate cancer.
Gene therapy and immune therapy
In the future, gene therapy or immune therapy may be successful in treating prostate cancer. Current technology limits the use of these experimental treatments to a small number of medical centers.
Prevention
Prostate cancer can't be prevented, but you can take measures to reduce your risk or possibly slow the disease's development.
* Eat well. High-fat diets have been linked to prostate cancer. Therefore, limiting your intake of high-fat foods and emphasizing fruits, vegetables and whole fibers may help you reduce your risk. Foods rich in lycopene, an antioxidant, also may help lower your prostate cancer risk. These foods include raw or cooked tomatoes, tomato products, grapefruit and watermelon. Garlic and some vegetables such as arugula, bok choy, broccoli, Brussels sprouts, cabbage and cauliflower also may help fight cancer. Vitamin E has shown promise in reducing the risk of prostate cancer among smokers. More research is needed, however, to see whether vitamin E might be effective.
* Get regular exercise. Regular exercise can help prevent a heart attack and conditions such as high blood pressure and high cholesterol. When it comes to cancer, the data aren't as clear-cut, but studies do indicate that regular exercise may reduce your cancer risk, including your risk of prostate cancer. Exercise has been shown to strengthen your immune system, improve circulation and speed digestion — all of which may play a role in cancer prevention. Exercise also helps to prevent obesity, another potential risk factor for some cancers. Regular exercise may also minimize your symptoms and reduce your risk of prostate gland enlargement, or benign prostatic hyperplasia (BPH). Men who are physically active usually have less-severe symptoms than do men who get little exercise.
* Ask your doctor about taking an NSAID. Nonsteroidal anti-inflammatory drugs (NSAIDs) might prevent prostate cancer. These drugs include ibuprofen (Advil, Motrin, others) and naproxen (Aleve). NSAIDs inhibit an enzyme called COX-2, which is found in prostate cancer cells. More studies are needed to confirm whether NSAID use actually results in lower rates of prostate cancer or reduced deaths from the disease.
Research on prostate cancer prevention has shown that the drug finasteride (Proscar, Propecia) may prevent or delay the onset of prostate cancer in men 55 years and older. This drug is currently used to control prostate gland enlargement and hair loss in men. However, finasteride has also been shown to contribute to increasing sexual side effects and to slightly raise the risk of developing higher grade prostate cancer. At this time, this drug isn't routinely recommended to prevent prostate cancer.
Coping and support
Once you receive a diagnosis of prostate cancer or treatment for this disease, you may experience a range of feelings — including disbelief, fear, anger, anxiety, emptiness and depression. You may not be able to get rid of these distressing feelings. But you can find positive ways to deal with them so they don't dominate your life. The following strategies can help you cope with some of the difficulties of prostate cancer:
* Be prepared. Ask your doctor questions and read about prostate cancer and its potential side effects. The fewer the surprises, the more quickly you'll adapt.
* Maintain as normal a routine as you can. Don't let the cancer or side effects from treatment dominate your day. Try to follow the routine and lifestyle you had before learning of your cancer. Go back to work, take a trip, join your children or grandchildren on an outing. You need activities that give you a sense of purpose, fulfillment and meaning. But realize that initially you may have some limitations. Start slowly and gradually build your level of endurance.
* Get plenty of exercise. Exercise helps fight depression and is a good way to relieve tension and aggression.
* Open up to a friend, a family member or a counselor. Cancer is too heavy a load to carry alone. Sometimes it helps to talk with someone about your feelings and fears. The better you feel emotionally, the better you'll be able to physically cope with your illness. You may find joining a support group helpful, because it can provide you with a sense of belonging, give you an opportunity to talk with people who understand your situation and provide you with advice. Your doctor or someone you know who has experienced prostate cancer may be able to help you locate a support group.
* Don't avoid sexual contact. Your natural reaction to impotence may be to avoid all sexual contact. Don't fall for this feeling. Touching, holding, hugging and caressing can become far more important to you and your partner. In fact, the closeness you develop in these actions can produce greater sexual intimacy than you've ever had before. There are many ways to express your sexuality.
* Look for the positive. Cancer doesn't have to be an all-negative experience for you. Good can come out of it. Confrontation with cancer may lead you to grow emotionally and spiritually, to identify what really matters to you, to settle long-standing disputes and to spend more time with people important to you.
Alternative medicine
A range of dietary supplements and herbal medicines claim to offer new ways to prevent or treat prostate disease, and cancer in general. Some supplements show promise and are slowly gaining acceptance in mainstream medicine. But the benefits and risks of many products and practices remain unproved. Unfortunately, the production of these products isn't well regulated, and the amount of active ingredient may vary from bottle to bottle or even pill to pill.
Herbal products marketed to relieve common prostate problems, such as frequent urination or a weak urine flow, include:
* African plum tree (Prunus africana)
* African wild potato (Hypoxis hemerocallidea, Hypoxis rooperi)
* Pumpkin (Cucurbita pepo)
* Rye grass (Secale cereale)
* Stinging nettle (Urtica dioica, Urtica urens)
Taken in small to moderate amounts, these products appear to be safe. But they haven't been studied in large, long-term trials to confirm their safety or to prove they work.
Saw palmetto
Unlike other herbal supplements, saw palmetto has been widely tested, and the results show promise in the treatment of urinary symptoms caused by prostate problems. However, it is important to know that saw palmetto is recommended to treat symptoms associated with benign prostate gland enlargement, not prostate cancer.
Saw palmetto works slowly. Most men begin to see an improvement in their urinary symptoms within one to three months. If after three months you haven't noticed any benefit from the product, it may not work for you. It appears safe to take saw palmetto indefinitely, but possible effects from long-term use are unknown. One drawback of this herb, and many other such herbal products, is that it may suppress PSA levels in your blood. This action can interfere with the effectiveness of the PSA test. That's why if you take saw palmetto or other herbal medicines, it's important to tell your doctor before having a PSA test.
Lacking scientific evidence
A few herbal and dietary products claim to help cure or prevent cancer. There's no scientific evidence that these products work, and some may be dangerous. Three popular "cancer-fighting" supplements include:
* Chaparral. Also known as creosote bush or greasewood, chaparral (Larrea tridentata) comes from a desert shrub found in the southwestern United States and Mexico. Research hasn't shown that the herb effectively treats cancer, and it can lead to irreversible liver failure.
* PC-SPES. This mixture contains eight herbs that have been used for hundreds of years in traditional Chinese medicine to treat prostate issues and other health problems. Some studies show it may reduce cancer growth, but it can also cause side effects. It was sold as a dietary supplement, but is no longer being manufactured because some batches were found to contain prescription drug ingredients. While the individual herbs are still available, the PC-SPES mixture has not been reintroduced because further studies are needed to determine whether it's safe.
* Shark cartilage. Shark cartilage contains a protein that has some ability to inhibit the formation of new blood vessels within tumors in sharks. Shark cartilage therapy is based on the theory that capsules containing shark cartilage will do the same in humans — stop and shrink cancerous tumors. However, these benefits haven't been shown in humans.
Talk with your doctor first
Because it's not always easy to tell which products may be unsafe, interact negatively with other medications or affect your overall cancer treatment, it's best to talk with your doctor before you take any dietary or herbal product.
Warning: The reader of this article should exercise all precautionary measures while following instructions on the home remedies from this article. Avoid using any of these products if you are allergic to it. The responsibility lies with the reader and not with the site or the writer.
The service is provided as general information only, and should not be treated as a substitute for the medical advice of your own doctor.



0 comments:
Post a Comment